
Use the arrows or click on the images to navigate the overview.
Underneath whoever we may think we are, before even the capacity for thought or feeling, we are human. We are animal. Rather than appealing to a "higher" or "better" self, we are dedicated to awakening a primal self, vibrant & explosively alive.
Join us on a journey from the corporeal to the existential and ignite the power of your own inner nature.
This is a method for healing, a path to self-discovery, and ultimately a way of life.
-
4-hour afternoon intensive that will introduce you to the power of hormesis. Follow-up call for accountability and integration.
Dec 20, 2022.
$125
Register here.
-
4.5-hour afternoon intensive designed to give effective and accessible tools to those grappling with addiction or recovery. One preparatory call and another for post-experience accountability and integration.
Dec 19, 2022
$125
Grants available for qualified participants.
Register here.
-
2-day immersive experience exploring the psychological and physiological dimensions of hormesis. For personal or professional application. Two preparatory calls and one for follow-up.
Dec 17-18, 2022
$500
Register here.
Use the arrows or click on the images to navigate the programs.
Ready to go?
Sign up here.
Want to learn more?
Read on below or set up a call here.
Want to be a sponsor?
Information for local organizations here.
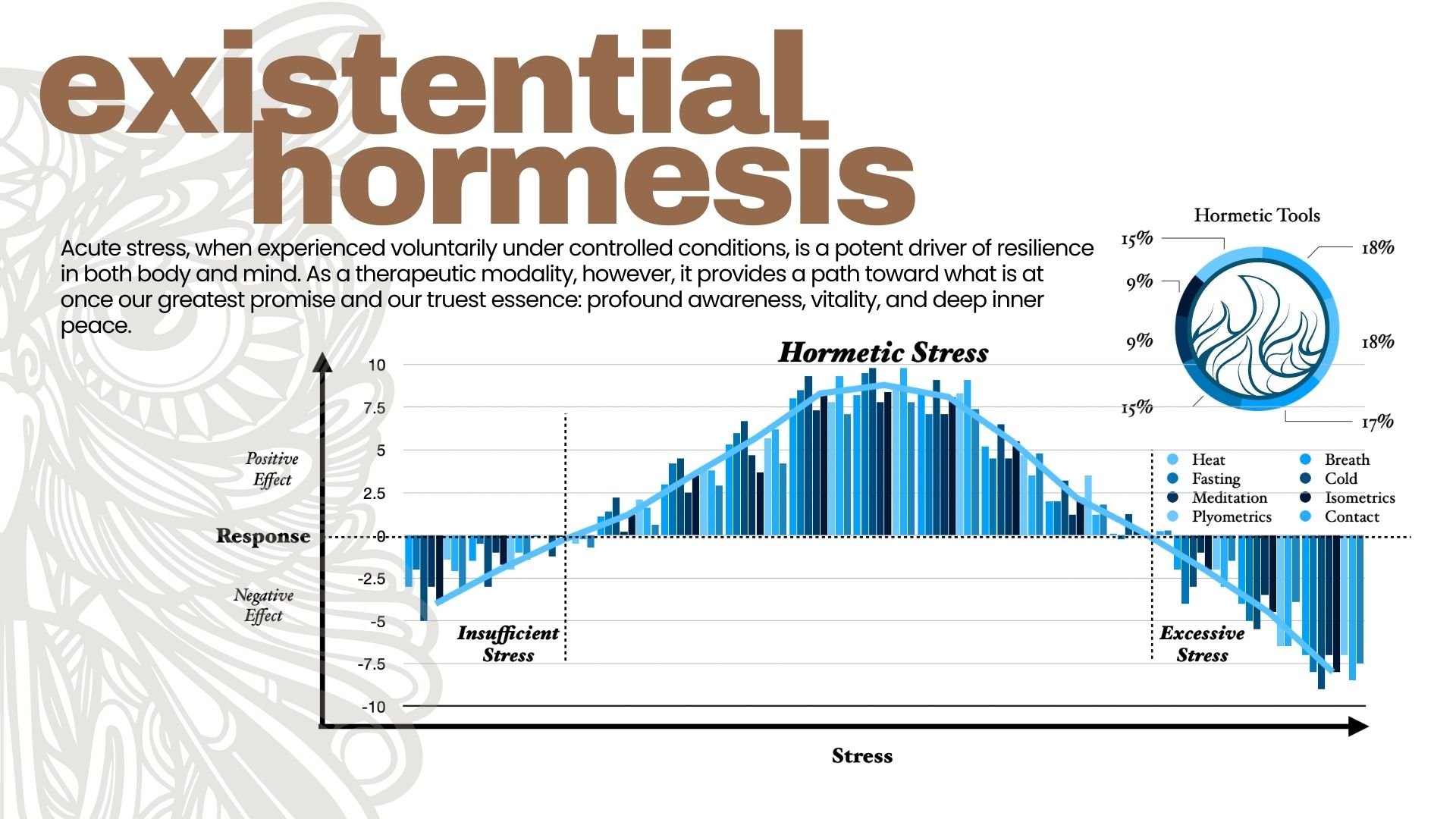
What is hormesis?
In simple terms, hormesis refers to the principle that acute stress, when experienced voluntarily under controlled conditions, is a potent driver of resilience in both body and mind. As a therapeutic modality, however, hormetic training can take us further into a state of profound awareness, vitality, and deep inner peace.
Hormetic training is a relatively new concept to western science, bridging what are often thought of as two separate realms: mental and physical health. Through simple protocols with readily available tools such as breathwork, cold exposure, and heat exposure, we can cultivate not just physiological resilience but mental clarity, connection, and emotional depth as well.
If you want to delve into research and scientific foundations of this approach we can begin by defining some basic concepts:
Hormesis
The term hormesis refers to how a typically toxic substance can have beneficial effects at low doses. This has been called the “dose-response revolution” (Calabrese 2003). “In the fields of biology and medicine hormesis is defined as an adaptive response of cells and organisms to a moderate (usually intermittent) stress” (Mattson 2008). The strategic implementation of intermittent stress, when administered appropriately, is an extremely effective way to heal and strengthen a wide range of physiological and neurological systems within the human body.
Homeostasis
Homeostasis is our goal as an organism, in all physiological and neurological systems; if our stress is too great, we cannot recover it. If stress is too little, however, we lose our natural ability to recover from even minor challenges. “Homeostasis is a kind of force ensuring that life is regulated within a range that is not just compatible with survival but also conducive to flourishing, to a projection of life into the future of an organism or a species” (Damasio 2018).
Allostasis
Allostasis, in essence, is our ability to respond to hormetic stressors in order to return to homeostasis. “Allostasis is the extension of the concept of homeostasis and represents the adaptation process of the complex physiological system to physical, psychosocial and environmental challenges or stress” (Logan 2008).
Allostatic load
Allostatic load refers to the tipping point, the amount of accumulated stress to which we are unable to respond productively. “Allostatic load is the long-term result of failed adaptation or allostasis, resulting in pathology and chronic illness” (Logan 2008).
Adaptive homeostasis
This refers to what is sometimes known as the “crossover effect,” whereby the ability to maintain or return to homeostasis in one biological system — for example thermoregulation — increases the body’s ability to maintain or return to homeostasis in another biological system — for example dopamine and seratonin levels in the brain (Pomatto 2017).
In short, hormesis is the therapeutic means by which we can increase our capacity for allostasis, thus allowing us to bear a heavier allostatic load for both physical and psychological stress. The end result is that our bodies and brains awaken their innate faculties of adaptive homeostasis.
As individuals and healthcare professionals we can learn to consistently return to homeostatic equilibrium in our physiology and neurology, even in the face of extreme and persistent stress.
What techniques or tools will we be learning?
When it comes to the actual impact of the experience, the best understanding comes through actually feeling it yourself. There’s only so much that can be measured and studied, and the subjective experience of vitality, balance, or inner peace have yet to be quantified in scientific terms. That said, there have been numerous studies showing the more easily measured benefits of hormesis.
Breath
Strategically applied breathwork protocols can have a profound affect on both acute and chronic conditions. The targeted cycling of high oxygen levels (hyperoxia) and low oxygen levels (hypoxia and hypoxemia), paired with corresponding low CO2 levels (hypercapnia) and low CO2 levels (hypocapnia) has been shown to increase longevity (Zubieta-Calleja 2017), strengthen the immune system (Harmke 2016), increase neuroplasticity (Wakhloo 2020), activate the parasympathetic nervous system (Fletcher 2000), and thereby play a fundamental role in the recovery from trauma and other acute conditions, most notably including depression and anxiety (Bloch 2021, Feng 2017, and Nazario 2011).
Cold
Exposure to conditions of extreme cold, when done in a safe and controlled setting with appropriate recovery times, has been shown to strengthen the immune system (Gill 2017), combat depression, anxiety, and a variety of other major psychological disorders including Schizophrenia (Briley 2011 and Jedema 2008), increase neuroplasticity and neurogenesis (Kim 2019), improve muscle function through increased mitochondrial biogenesis (Memme 2019 and Sun 2016), decrease recovery times from both exercise and acute physical trauma (Banfi 2009 and Pournot 2011), and decrease inflammation whether chronic or acute (Lin 2020 and Pongratz 2014). It provides effective treatment for a wide variety of disease caused by autoimmune disfunction, ranging from Type 2 diabetes to rheumatoid arthritis (Dulloo 2013 and Lin 2020), as well as neurodegenerative conditions such as Alzheimer’s and Parkinson’s disease (Jackson 2015 and Tsai 2020). It also increases metabolism and improves the gut microbiome (Blondin 2014 and Chevalier 2015), making it an incredibly powerful tool in the hormetic toolkit.
Heat
The appropriate and strategic use of intense heat exposure has been demonstrated to have wide-ranging benefits for both physical and mental health. Following a specific protocol of sauna use, for example, has been shown to reduce the development psychotic disorders by a full 77%, regardless of dietary habits, socioeconomic status, physical activity, and inflammatory status (Laukkanen 2017). These same studies showed a 66% lower risk of developing dementia and a 65% lower risk of developing Alzheimer's disease (Laukkanen 2017). It has also been shown to speed the recovery of traumatic brain injury (Umschweif 2013), and decrease all-cause mortality by 40% (Laukkanen 2015). It has been shown to provide an effective treatment for depression and other mood disorders (Janssen 2016), improve mental focus and attention in both adults and children (Wigal 2003), as well as increase metabolism (Kokura 2007) and aid significantly in gaining strength and physical endurance (Scoon 2007).
Our aim is to provide a theoretical framework for understanding the mechanisms and benefits, as well as the practical experience necessary to use these tools safely and effectively.
References
Banfi, Giuseppe, Gianluca Melegati, Alessandra Barassi, Giada Dogliotti, Gianvico Melzi d’Eril, Benoit Dugué, and Massimiliano M. Corsi. Effects of whole-body cryotherapy on serum mediators of inflammation and serum muscle enzymes in athletes. Journal of Thermal Biology 34, no. 2 (February 2009): 55–59. https://doi.org/10.1016/j.jtherbio.2008.10.003.
Bloch, Y., Belmaker, R.H., Shvartzman, P. et al. Normobaric oxygen treatment for mild-to-moderate depression: a randomized, double-blind, proof-of-concept trial. Sci Rep 11, 18911 (2021). https://doi.org/10.1038/s41598-021-98245-9
Blondin, Denis P., Sébastien M. Labbé, Hans C. Tingelstad, Christophe Noll, Margaret Kunach, Serge Phoenix, Brigitte Guérin, et al. Increased Brown Adipose Tissue Oxidative Capacity in Cold-Acclimated Humans. The Journal of Clinical Endocrinology & Metabolism 99, no. 3 (March 2014): E438–E446. https://doi.org/10.1210/jc.2013-3901.
Briley, Mike, and Moret Chantal. The importance of norepinephrine in depression, Neuropsychiatric Disease and Treatment, May 2011, 9. https://doi.org/10.2147/ndt.s19619.
Calabrese, E. J., & Baldwin, L. A. (2003). Hormesis: the dose-response revolution. Annual review of pharmacology and toxicology, 43, 175–197. https://doi.org/10.1146/annurev.pharmtox.43.100901.140223
Chevalier, Claire, Ozren Stojanović, Didier J. Colin, Nicolas Suarez-Zamorano, Valentina Tarallo, Christelle Veyrat-Durebex, Dorothée Rigo, et al. Gut Microbiota Orchestrates Energy Homeostasis during Cold Cell 163, no. 6 (December 2015): 1360–74. https://doi.org/10.1016/j.cell.2015.11.004.
Damasio AR. The Strange Order of Things. Life, Feeling, and the Making of Cultures. New York: Pantheon Books, 2018. [Google Scholar] [Ref list]
Dulloo, Abdul G. Translational issues in targeting brown adipose tissue thermogenesis for human obesity management Annals of the New York Academy of Sciences 1302, no. 1 (October 2013): 1–10. https://doi.org/10.1111/nyas.12304.
Feng JJ, Li YH. Effects of hyperbaric oxygen therapy on depression and anxiety in the patients with incomplete spinal cord injury (a STROBE-compliant article). Medicine (Baltimore). 2017 Jul;96(29):e7334. doi: 10.1097/MD.0000000000007334. PMID: 28723746; PMCID: PMC5521886.
Fletcher E. C. (2000). Effect of episodic hypoxia on sympathetic activity and blood pressure. Respiration physiology, 119(2-3), 189–197. https://doi.org/10.1016/s0034-5687(99)00114-0
Gill, J.A., and Michele A. La Merrill. An emerging role for epigenetic regulation of Pgc-1 expression in environmentally stimulated brown adipose thermogenesis Environmental Epigenetics 3, no. 2 (May 2017). https://doi.org/10.1093/eep/dvx009.
Harmke D. Kiers, Gert-Jan Scheffer, Johannes G. van der Hoeven, Holger K. Eltzschig, Peter Pickkers, Matthijs Kox; Immunologic Consequences of Hypoxia during Critical Illness. Anesthesiology 2016; 125:237–249 doi: https://doi.org/10.1097/ALN.0000000000001163
Jackson, T.C., M.D. Manole, S.E. Kotermanski, E.K. Jackson, R.S.B. Clark, and P.M. Kochanek. Cold stress protein RBM3 responds to temperature change in an ultra-sensitive manner in young neurons Neuroscience 305 (October 2015): 268–78. https://doi.org/10.1016/j.neuroscience.2015.08.012.
Janssen, Clemens W., Christopher A. Lowry, Matthias R. Mehl, John J. B. Allen, Kimberly L. Kelly, Danielle E. Gartner, Angelica Medrano, et al. Whole-Body Hyperthermia for the Treatment of Major Depressive Disorder JAMA Psychiatry 73, no. 8 (August 2016): 789. doi:10.1001/jamapsychiatry.2016.1031.
Jedema, Hank P., Stephen J. Gold, Guillermo Gonzalez-Burgos, Alan F. Sved, Ben J. Tobe, Theodore G. Wensel, and Anthony A. Grace. Chronic cold exposure increases RGS7 expression and decreases 2-autoreceptor-mediated inhibition of noradrenergic locus coeruleus neurons European Journal of Neuroscience 27, no. 9 (April 2008): 2433–43. https://doi.org/10.1111/j.1460-9568.2008.06208.x.
Kim, J. W., Han, K. R., Kim, W., Jung, H. Y., Nam, S. M., Yoo, D. Y., Hwang, I. K., Seong, J. K., & Yoon, Y. S. (2019). Adult Hippocampal Neurogenesis Can Be Enhanced by Cold Challenge Independently From Beigeing Effects. Frontiers in neuroscience, 13, 92. https://doi.org/10.3389/fnins.2019.00092
Kokura, Satoshi, Satoko Adachi, Emiko Manabe, Katsura Mizushima, Takeshi Hattori, Toshimitsu Okuda, Nami Nakabe, et al. Whole body hyperthermia improves obesity-induced insulin resistance in diabetic mice International Journal of Hyperthermia 23, no. 3 (January 2007): 259–65. doi:10.1080/02656730601176824.
Laukkanen, Tanjaniina, Hassan Khan, Francesco Zaccardi, and Jari A. Laukkanen. Association Between Sauna Bathing and Fatal Cardiovascular and All-Cause Mortality Events JAMA Internal Medicine 175, no. 4 (April 2015): 542. doi:10.1001/jamainternmed.2014.8187.
Laukkanen, Tanjaniina, Setor Kunutsor, Jussi Kauhanen, Jari Antero Laukkanen Sauna bathing is inversely associated with dementia and Alzheimer's disease in middle-aged Finnish men Age Ageing . 2017 Mar 1;46(2):245-249
Lin, Yen-Ju, Martina Anzaghe, and Stefan Schülke. Update on the Pathomechanism, Diagnosis, and Treatment Options for Rheumatoid Arthritis Cells 9, no. 4 (April 2020): 880. https://doi.org/10.3390/cells9040880.
Logan, J. G., & Barksdale, D. J. (2008). Allostasis and allostatic load: expanding the discourse on stress and cardiovascular disease. Journal of clinical nursing, 17(7B), 201–208. https://doi.org/10.1111/j.1365-2702.2008.02347.x
Mattson M. P. (2008). Hormesis defined. Ageing research reviews, 7(1), 1–7. https://doi.org/10.1016/j.arr.2007.08.007
Memme, Jonathan M., Avigail T. Erlich, Geetika Phukan, and David A. Hood. Exercise and mitochondrial health The Journal of Physiology 599, no. 3 (December 2019): 803–17. https://doi.org/10.1113/jp278853.
McEwen, B. S., & Gianaros, P. J. (2011). Stress- and allostasis-induced brain plasticity. Annual review of medicine, 62, 431–445. https://doi.org/10.1146/annurev-med-052209-100430
Nazario, J., & Kuffler, D. P. (2011). Hyperbaric oxygen therapy and promoting neurological recovery following nerve trauma. Undersea & hyperbaric medicine : journal of the Undersea and Hyperbaric Medical Society, Inc, 38(5), 345–366.
Pomatto, Laura, and Kelvin J.A. Davies. The role of declining adaptive homeostasis in ageing. The Journal of Physiology 595, no. 24 (October 2017). https://doi.org/10.1113/JP275072
Pongratz, Georg, and Rainer H Straub. The sympathetic nervous response in inflammation. Arthritis Research & Therapy 16, no. 6 (December 2014). https://doi.org/10.1186/s13075-014-0504-2.
Pournot, Hervé, François Bieuzen, Julien Louis, Jean-Robert Fillard, Etienne Barbiche, and Christophe Hausswirth. Time-Course of Changes in Inflammatory Response after Whole-Body Cryotherapy Multi Exposures following Severe Exercise PLoS ONE Edited by Alejandro Lucia. 6, no. 7 (July 2011): e22748. https://doi.org/10.1371/journal.pone.0022748.
Scoon, Guy S.M., William G. Hopkins, Simon Mayhew, and James D. Cotter. Effect of post-exercise sauna bathing on the endurance performance of competitive male runners Journal of Science and Medicine in Sport 10, no. 4 (August 2007): 259–62. doi:10.1016/j.jsams.2006.06.009.
Shevchuk, Nikolai. (2008). Adapted cold shower as a potential treatment for depression. Medical hypotheses. 70. 995-1001. 10.1016/j.mehy.2007.04.052.
Sun, Nuo, Richard J. Youle, and Toren Finkel. The Mitochondrial Basis of Aging Molecular Cell 61, no. 5 (March 2016): 654–66. https://doi.org/10.1016/j.molcel.2016.01.028.
Tsai Yi-Ju, Jhong Yue-Cih, Ching Shih-Hong, Liao Yu-Ching, Ching Cheng-Hsin, Chuang Jih-Ing. Cold Exposure After Exercise Impedes the Neuroprotective Effects of Exercise on Thermoregulation and UCP4 Expression in an MPTP-Induced Parkinsonian Mouse Model. Frontiers in Neuroscience, 14. 2020. doi: 10.3389/fnins.2020.573509
Umschweif G, Alexandrovich AG, Trembovler V, Horowitz M, Shohami E. Hypoxia-inducible factor 1 is essential for spontaneous recovery from traumatic brain injury and is a key mediator of heat acclimation induced neuroprotection. J Cereb Blood Flow Metab. 2013 Apr;33(4):524-31. doi: 10.1038/jcbfm.2012.193. Epub 2013 Jan 2. PMID: 23281425; PMCID: PMC3618386.
Wakhloo, D., Scharkowski, F., Curto, Y. et al. Functional hypoxia drives neuroplasticity and neurogenesis via brain erythropoietin. Nat Commun 11, 1313 (2020). https://doi.org/10.1038/s41467-020-15041-1
Wigal, Sharon B, Dan Nemet, James M Swanson, Roland Regino, Joey Trampush, Michael G Ziegler, and Dan M Cooper. Catecholamine Response to Exercise in Children with Attention Deficit Hyperactivity Disorder Pediatric Research 53, no. 5 (May 2003): 756–61. doi:10.1203/01.pdr.0000061750.71168.23.
Zubieta-Calleja, Gustavo & Zubieta-DeUrioste, Natalia. (2017). Extended Longevity at high altitude: Benefits of exposure to Chronic Hypoxia. BLDE Journal of Health Sciences. 2. 80-90.
